
January is Cervical Cancer Awareness month. Together we can raise the awareness of cervical cancer and cure the disease that is curable and preventable.
What Is Cervical Cancer?
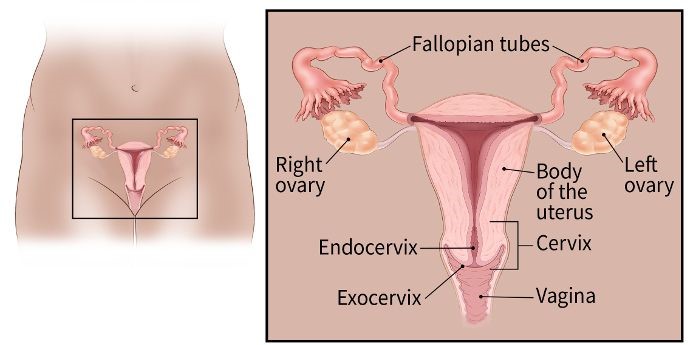
Cervical cancer starts in the cells lining the cervix -- the lower part of the uterus (womb). The cervix connects the body of the uterus (the upper part where a fetus grows) to the vagina (birth canal).
The cervix is made of two parts and is covered with two different types of cells.
- The endocervix is the opening of the cervix that leads into the uterus. It is covered with glandular cells.
- The exocervix (or ectocervix) is the outer part of the cervix that can be seen by the doctor during a speculum exam. It is covered in squamous cells.
The place where these two cell types meet in the cervix is called the transformation zone. The exact location of the transformation zone changes as you get older and if you give birth. Most cervical cancers begin in the cells in the transformation zone.
Source: https://www.cancer.org/cancer/cervical-cancer/about/what-is-cervical-cancer.html
What is Cervical Screening?
The goal of cervical cancer screening is to find pre-cancer or cancer early when it is more treatable and curable. Regular screening can prevent cervical cancers and save lives. The tests for cervical cancer screening are the HPV test and the Pap test.
- Cervical cancer testing (screening) should begin at age 25.
- Those aged 25 to 65 should have a primary HPV test* every 5 years. If primary HPV testing is not available, screening may be done with either a co-test that combines an HPV test with a Papanicolaou (Pap) test every 5 years or a Pap test alone every 3 years.
- The most important thing to remember is to get screened regularly, no matter which tests you get
- Those over age 65 who have had regular screening in the past 10 years with normal results and no history of CIN2 or more serious diagnosis within the past 25 years should stop cervical cancer screening. Once stopped, it should not be started again.
- People who have had a total hysterectomy (removal of the uterus and cervix) should stop screening (such as Pap tests and HPV tests) unless the hysterectomy was done as a treatment for cervical cancer or serious pre-cancer. People who have had a hysterectomy without removal of the cervix (called a supracervical hysterectomy) should continue cervical cancer screening according to the guidelines above
- People who have been vaccinated against HPV should still follow these guidelines for their age groups.
Check out the Bioperfectus HPV testing solution here.
References:

